Introduction
HIPAA compliance is not just a checklist; it’s a day-to-day dedication to patient safety, privacy, and trust. Regardless if you’re a physician, nurse, practice manager, or third-party vendor, you work with information patients expect you to guard.
In this manual, we will lay out exactly what HIPAA compliance is, why it’s so important in the modern healthcare system, and the precise steps you can follow to achieve compliance. By the end of it, you’ll be familiar with your obligations and have the resources to maintain compliance on a daily basis.
What Is HIPAA Compliance?
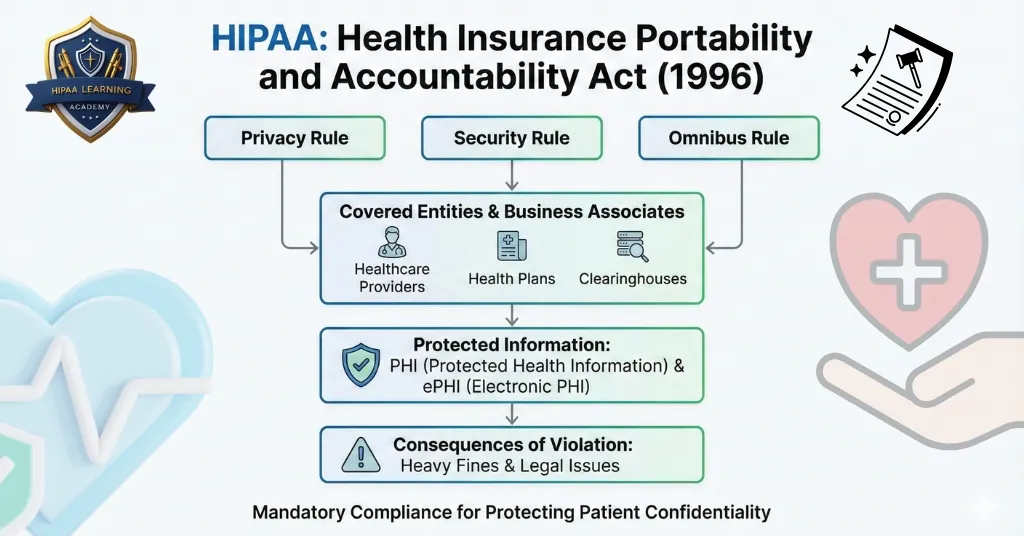
HIPAA is an acronym for the Health Insurance Portability and Accountability Act, a 1996 federal law that ensures the security and privacy of confidential patient information.
Compliance entails adhering to all applicable laws when gathering, storing, transmitting, and discarding Protected Health Information (PHI). PHI is any piece of information capable of identifying a patient, whether it is in paper records, electronic records, or even verbal communication.
A few examples of PHI are:
- Patient names and addresses, Even simple contact information is sensitive and requires protection.
- Medical records and diagnoses, Information regarding illnesses, treatments, and test results must be kept confidential.
- Payment and insurance information, Policy numbers, payment history, and claims information are all part of PHI.
- Lab test results, These tend to include both patient identifiers and health information.
- Any information that can be used to identify a patient, This may include photographs, biometric information, or appointment information.
Why HIPAA Compliance is Important in 2025

The risk to patient data has never been more significant. With telehealth and electronic health records on the rise, PHI is more than ever in electronic storage and in circulation. Both legally and strategically, compliance is more important than ever before.
What’s critical about HIPAA compliance:
- Maintains patient confidentiality and trust, Patients will be more willing to provide the correct information if they believe their information is secure.
- Avoids expensive fines and legal action, Failure to comply can cost millions and even result in legal action against you.
- Reduces liability for data breaches and hacking, Robust security minimizes potential for invasion.
- Preserves professional image, A breach of privacy will harm your reputation among the healthcare professional community.
- Satisfies federal legal requirements, HIPAA compliance is not a choice, but rather a matter of law for covered entities and business associates.
The Core HIPAA Rules You Should Know
1. Privacy Rule
The Privacy Rule is the basis for HIPAA compliance, as it dictates who can have access to Protected Health Information (PHI) and under what conditions. It gives patients a lot of control over their health information, such as the right to obtain copies of their medical records, examine them, and even demand corrections if they find mistakes.
This provision aims to stop unauthorized parties, organizations, or even healthcare personnel from viewing and divulging patient data without valid reason. Exceptions are permitted for vital purposes like treatment, payment, or healthcare operations, but anything more than these must be authorized by the patient.
By adopting the Privacy Rule, healthcare providers not only adhere to the law but also gain enhanced patient trust since individuals feel safe with their own health information being treated responsibly.
2. Security Rule
The Security Rule deals particularly with the protection of electronic PHI (ePHI). With most healthcare information today being electronically stored and transmitted, the Security Rule plays a central role in guarding against data breaches and cyberattacks.
It calls for healthcare organizations to institute administrative, technical, and physical safeguards.
- Administrative safeguards include employees’ training, the designation of security roles, and applying risk management procedures.
- Technical safeguards include encryption, firewalls, multi-factor authentication, and safe transmission channels to protect data confidentiality.
- Physical safeguards describe measures like locked file rooms, access constraints to the data server, and surveillance systems to avoid unauthorized access.
By implementing these protections, healthcare providers design several layers of security around confidential patient information, limiting the potential for exposure while fortifying organizational security measures.
3. Breach Notification Rule
The Breach Notification Rule specifies how healthcare providers and business associates are required to act in the unfortunate event of a data breach. When PHI is compromised, organizations have to immediately notify the affected individuals so that they know their privacy might be at risk.
In addition to individual notice, the Department of Health and Human Services (HHS) also has to be notified, and in case the breach affects over 500 individuals, local news media must also be informed. This way, breaches are not concealed or delayed but are addressed openly.
Timely notification is required not only for legal reasons but also to support patient trust. Patients have the right to be notified when their information has been breached so that they can take precautionary measures, including monitoring accounts for identity theft. This rule emphasizes responsibility, since healthcare organizations must own up to data security failures and act rapidly to reduce damage.
4. Rule of Enforcement
The Enforcement Rule provides the framework for investigating, enforcing, and penalizing HIPAA violations. The Office for Civil Rights (OCR) under the Department of Health and Human Services has the responsibility of oversight.
In case of a violation, investigations, audits, or reviews can be conducted by the OCR to determine the breach’s severity. Depending upon the results, penalties can vary from financial fines to required corrective action plans, which guarantee that the organization takes steps to fill compliance loopholes.
In instances of intentional neglect or ill will, the OCR can refer the case to criminal prosecution, which may result in both fines and jail time. The Enforcement Rule makes it explicit that HIPAA compliance is not optional and that non-compliance carries significant penalties. It emphasizes the need for accountability across all levels of healthcare operations and ensures organizations remain vigilant in safeguarding patient information.
Who is HIPAA Compliant Required To Be?
HIPAA governs two primary groups: covered entities and business associates.
Covered entities are:
- Hospitals and clinics, Any healthcare facility that provides healthcare services to patients.
- Doctors and dentists, Private practice, specialists, and general practitioners.
- Insurance companies for healthcare, Organizations that pay medical claims and benefits.
- Pharmacies, Companies that maintain and process prescription data.
Business associates are:
- Medical billing firms, Manage insurance claims and patient payment information.
- IT service providers that deal with PHI, Manage electronic health record systems or data storage.
- Transcription services, Record patient notes in written or electronic form.
- Third-party administrators, Offer administrative support for healthcare providers.
If your job entails accessing, processing, or storing PHI in any way, HIPAA compliance is mandated.
HIPAA Compliance Requirements

The process of being HIPAA compliant is continuous. The following are the requirements that every healthcare professional must adhere to:
- Train employees on HIPAA regulations, Regular training ensures that all employees know what PHI is, how to work with it, and what happens when it is mishandled.
- Protect PHI with safeguards, These encompass encryption for electronic records, locked files for paper documents, and password-protected systems.
- Establish written policies, Your policies must outline precisely how PHI is gathered, accessed, disclosed, and destroyed.
- Execute Business Associate Agreements (BAAs), Any contractor dealing with PHI on your behalf must sign a BAA affirming their compliance.
- Perform routine risk assessments, Discover and repair vulnerabilities in your systems before they cause breaches.
Common HIPAA Violations
Even minor errors can constitute violations. Being aware of the most prevalent ones will prevent you from making them:
- Sharing PHI inappropriately, This means speaking about a patient in areas that are not supposed to be kept private or emailing unencrypted messages with PHI.
- Losing devices containing PHI, Laptops, phones, and USB storage devices containing PHI need to be encrypted and physically protected.
- Talking about patient cases openly, Hallways, elevators, and cafeterias do not qualify as private areas.
- Not logging out of systems, Leaving PHI on view on an unattended computer exposes data to risk.
- Late reporting of breaches, Failure to notify within the deadline will attract stiffer penalties.
Penalties for Non-Compliance
Penalties are based on the nature and intent of the breach:
- Fines of between $100 to $50,000 per violation, Minor infractions may be penalized at the lower end, but repeated or deliberate breaches are expensive.
- Annual maximum of $1.5 million, Organizations with multiple violations in a year can face this cap.
- Criminal charges, In cases of intentional misuse of PHI, individuals can face jail time.
- Loss of license or certification, Severe violations can impact professional standing and the ability to operate.
How to Stay HIPAA Compliant

The best way to stay compliant is to make HIPAA part of your daily routine:
- Conduct HIPAA training annually, Stay current with regulations and best practices for your employees.
- Encrypt all patient information, Encryption is like strong locks on a vault: even if someone gets past them, they can’t get inside.
- Restrict access to PHI, Only approved staff should see patient information, and only as needed.
- Keep audit trails, Keep close records of who looked at PHI and when they did.
- Review policies regularly, Laws and technology evolve, so look at your compliance policies at least once a year.
HIPAA Compliance Checklist for Health Care Professionals
Unless you can check off these items, don’t think of your organization as compliant yet:
- Employees trained within the past 12 months, Annual refresher keeps compliance foremost in mind.
- Policies written, Cover each phase of PHI handling.
- Secure disposal and storage, Shred paper files and securely delete electronic records.
- Strong passwords and encryption, Secure systems from unwanted access.
- Business Associate Contracts executed, Document compliance of all external partners.
- Risk assessments performed, Periodically discover and correct security vulnerabilities.
Resources and Further Reading
- S. Department of Health & Human Services HIPAA Overview
- HIPAA Learning Academy’s HIPAA Training Courses
Conclusion
HIPAA compliance isn’t a one-and-done task, it’s a continued responsibility that touches every area of patient care. Through knowledge of the rules, staff training, and robust safeguards, you’re not only complying with the law, but you’re reinforcing patient trust as well.
To be prepared for 2025 and beyond, review our HIPAA training options and empower your staff to safeguard patient privacy each day. For billing-related training, follow the Guardian Courses.





3 Responses