Introduction
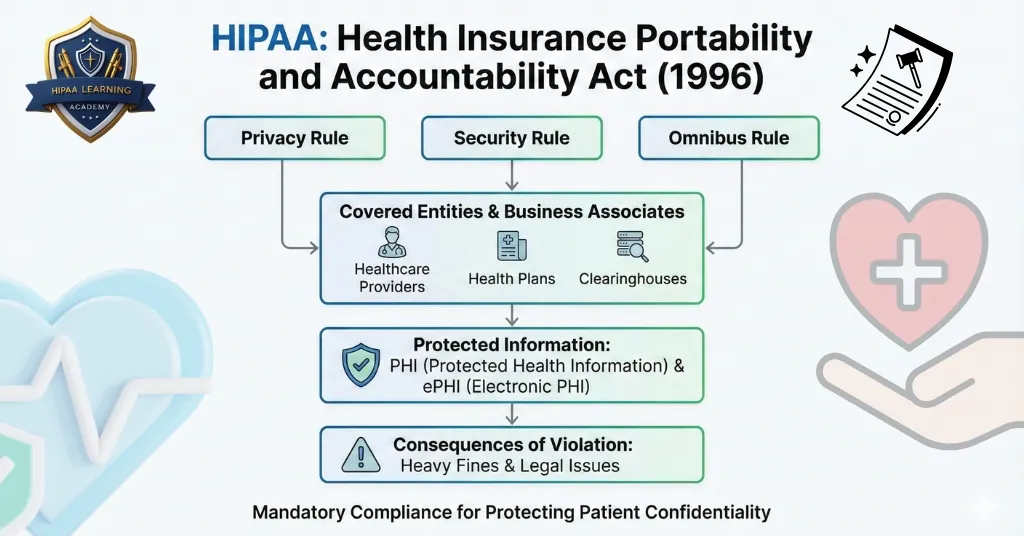
HIPAA compliance is not a collection of rules, it’s the basis of patient and provider trust. And yet, annually thousands of infractions are reported to the Office for Civil Rights (OCR), many of which could have been prevented with proper training and safeguards.
In this guide, we’ll look at the most prevalent HIPAA violations in 2025, why they are happening, the penalties they can result in, and most importantly, how you can prevent them in your organization. If you’re a healthcare provider, administrator, or business associate, knowing these violations is step one toward long-term compliance.
Why Understanding HIPAA Violations Matters in 2025

The healthcare industry is evolving rapidly, with more patient data stored and shared electronically than ever before. This digital shift brings both opportunities and risks. A single violation can damage your reputation, cost thousands, or even millions, in fines, and erode patient trust.
Key reasons to focus on prevention:
- Protecting patients’ privacy and dignity
- Reducing legal and financial risks
- Maintaining compliance with federal regulations
- Building a culture of security within your organization
Top Most Common HIPAA Violations of 2025

Inappropriate Access to Patient Records
Inappropriate access to a patient’s file without a legitimate work-related purpose is the most common type of reported breach. This may occur when employees access their friends’, family members’, or even celebrities’ records out of curiosity.
Why it’s an issue: It is an infringement on the HIPAA Privacy Rule and undermines patient trust.
Example: A hospital employee accessing a neighbor’s test results without being involved in their care.
How to avoid:
- Implement role-based access controls so employees can only view records necessary for their job.
- Regularly review audit logs to detect unauthorized access.
- Provide clear training on appropriate and inappropriate access.
Failing to Encrypt or Secure Patient Data
HIPAA’s Security Rule mandates protection for electronic PHI (ePHI) using methods such as encryption. If devices or servers on which patient information is stored are not properly secured, the risk of breaches is high.
Why it’s a problem: A stolen, unencrypted laptop could breach thousands of patient records.
Example: A clinic loses an unencrypted portable hard drive with sensitive data.
How to avoid:
- Encrypt all devices and data storage systems.
- Utilize secure, HIPAA-compliant cloud storage for backups.
- Enforce strong passwords and multi-factor authentication on all accounts.
Inadequate Disposal of PHI
Dumping medical records in public garbage cans or not correctly wiping old equipment can cause unauthorized access. Paper and electronic records need secure disposal procedures.
Why it’s an issue: Inadequate disposal will lead to PHI being accessed and misused.
Example: A dental office tosses patient files into a public dumpster.
How to prevent:
- Use cross-cut shredders to destroy paper records.
- Use certified e-waste disposal services for electronics.
- Maintain disposal procedures in a written HIPAA policy.
Employee HIPAA Training is Lacking
Most HIPAA violations occur because employees simply don’t understand what’s required. Without training, employees can accidentally mishandle PHI or fall prey to phishing schemes.
Why it’s a problem: Untrained employees are more likely to make expensive mistakes.
Example: A receptionist sends an unencrypted e-mail with PHI to an incorrect address.
How to prevent:
- Hold annual HIPAA training for all employees.
- Offer refresher training whenever laws are updated.
- Add real-world examples to training to make lessons applicable.
Not Granting Patients Access to Their Records
Under HIPAA, patients are entitled to access their medical records in a timely manner. Refusals or delays are a violation, even if not intentional.
Why it’s a problem: Denying access violates patient rights and can lead to legal action.
Example: A clinic takes months to respond to a patient’s record request.
How to avoid:
- Create a standardized process for fulfilling access requests.
- Train staff on required response timeframes (typically within 30 days).
- Use patient portals to streamline access.
Data Breach Notification Failures
If there is a breach, HIPAA’s Breach Notification Rule mandates timely notification to the affected parties, the OCR, and in some cases, the media. A failure to notify within the prescribed time frame constitutes an independent violation.
Why it’s a problem: Delay causes more harm and more penalties.
Example: A health clinic takes three months to report a breach that involved hundreds of patients.
How to avoid:
- Prepare a written breach response plan.
- Appoint a compliance officer to deal with notifications.
- Empower staff to report suspected violations as soon as possible.
Insecure Communication Channels
Transmitting PHI over unsecured text messages, personal email accounts, or non-compliant apps is a violation.
Why it’s an issue: These channels might be intercepted or accessed by unauthorized individuals.
Example: A nurse sends lab findings to a physician via a personal messaging app.
How to prevent:
- Utilize HIPAA-compliant messaging and email services.
- Ban utilization of personal devices for PHI unless they pass security testing.
- Encrypt all data being transmitted.
Penalties for HIPAA Violations in 2025
The OCR weighs intent, harm done, and corrective action taken when assessing penalties.
Possible sanctions include:
- Financial penalties between $100 and $50,000 per violation
- Annual maximum penalties of up to $1.5 million for repeated offenses
- Corrective action plans subject to constant monitoring
- Criminal prosecution in cases of intentional misconduct
- Loss of business reputation and patient trust
How to Prevent HIPAA Violations in 2025
Conduct Regular Risk Assessments
Identify your own weaknesses in systems and procedures before they lead to breaches. Document the findings and fix-it steps to remain proactive. Routine risk analysis not only points out vulnerabilities, but it also provides you with a road map of how to implement improved safeguards. By examining your processes on a regular basis, you can avoid expensive errors and maintain constant HIPAA compliance.
Keep Written Policies and Procedures
Clearly define how PHI may be accessed, stored, shared, and destroyed. Update policies in accordance with evolving technology and regulations. Written policies help ensure consistency throughout your organization and establish explicit expectations for your staff. They are also essential documentation of compliance in the event of an OCR audit, shielding your practice from unwarranted penalties.
Provide Ongoing Employee Training
Make HIPAA training a part of the onboarding and follow it up with annual refresher training. Incorporate phishing awareness and scenario-based exercises to enhance comprehension. Training must be practical and based on real-world situations from which your employees can relate. The more confident your staff will be dealing with PHI, the less likelihood of accidental violations or breaches.
Secure All Devices and Networks
Implement encryption, firewalls, secure Wi-Fi, and mobile device management software. Lock devices when not in use to avoid unauthorized access. Locking devices and networks minimizes the likelihood of cyberattacks and lost data. With remote work on the increase, ensuring mobile security and access control is more critical than ever.
Monitor and Audit Access Logs
Periodically scan system logs to make sure PHI is accessed by authorized personnel only. Watching for suspicious activity minimizes delays in finding a problem and allows you to correct it before it gets out of hand. Preemptive audits also create a sense of accountability among employees, so they know that patient information is being closely monitored and guarded.
Have a Breach Response Plan
Know precisely what to do in the event of a breach, such as notification and documentation timelines. A properly documented plan allows your staff to act rapidly without hesitation. Assigning definite responsibilities and practicing breach scenarios helps minimize downtime, limit damage, and preserve patient trust in sensitive circumstances.
HIPAA Compliance Checklist for 2025
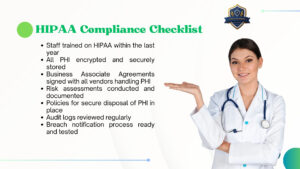
- Staff HIPAA-trained in the past year
- All PHI encrypted and safely archived
- Business Associate Agreements with all vendors that come into contact with PHI
- Risk assessments done and documented
- Secure disposal of PHI policies in place
- Audit logs checked on a regular basis
- Breach notification process set and tested
Resources and Further Reading
- U.S. Department of Health & Human Services HIPAA Overview
- HIPAA Learning Academy’s HIPAA Training Programs (internal link suggestion: /courses/hipaa-compliance-training)
Conclusion
HIPAA breaches can occur in any organization, but they are avoidable. By knowing the most prevalent errors and putting protections in place, you can safeguard patient privacy, stay compliant, and avoid financial penalties.
It is time to audit your policies, train your employees, and fortify your systems. In the fluid world of healthcare, prevention is not only better than a cure, it’s a must. For reliable training and continuous updates, explore resources like HIPAA Learning Academy and Guardian Dental Billing Trainings to ensure your team stays compliant and well-prepared.






One Response
loved it..